– Written by Dr Sarah Langton BVSc BVetBiol GradDipEd
What is pancreatitis?
Pancreatitis translates to ‘inflammation of the pancreas’. The pancreas is a glandular organ that nestles under the stomach and along the duodenum. The healthy pancreas has 2 main jobs, firstly to secrete digestive enzymes that help break down the nutrients your dog eats, the second job is to secrete insulin and glucagon (hormones that regulate the utilisation of these nutrients). The digestive enzymes are normally stored safely as inactive forms within pancreatic granules. In pancreatitis these enzymes are activated early before reaching the small intestine and they instead begin digesting the pancreas. This causes a lot of inflammation and damage to the pancreas.
What causes pancreatitis?
Although the inciting cause of pancreatitis is often unknown, in most cases it can be due to the following:
- Hormonal imbalance (e.g. diabetes mellitus or hypothyroidism)
- Certain medications
- Trauma to pancreas
- Pancreatic tumour
- Sudden high fat meal
- Reflux of digestive contents into pancreatic duct
What are the signs of pancreatitis?

Figure 1: A 6 month old female border collie named Raven having an examination with the vet and checking the abdomen for signs of pain.
There are two forms of pancreatitis; acute (quick and severe) or chronic (slow and mild). If your dog has acute pancreatitis, they typically have signs of vomiting, diarrhoea, a painful abdomen, and possibly a high temperature.
These signs are an emergency and your dog should be taken to a veterinarian immediately. Many complications can develop from acute pancreatitis, and the success of treatment depends on an early diagnosis.
A dog with chronic pancreatitis may have very mild signs such as having a reduced appetite, being quiet, and disinterested.
It is worth noting that the signs of pancreatitis are not specific and could be caused by other diseases, so it is crucial to diagnose or exclude pancreatitis so that your dog can receive the most effective treatment possible.
How is pancreatitis diagnosed?
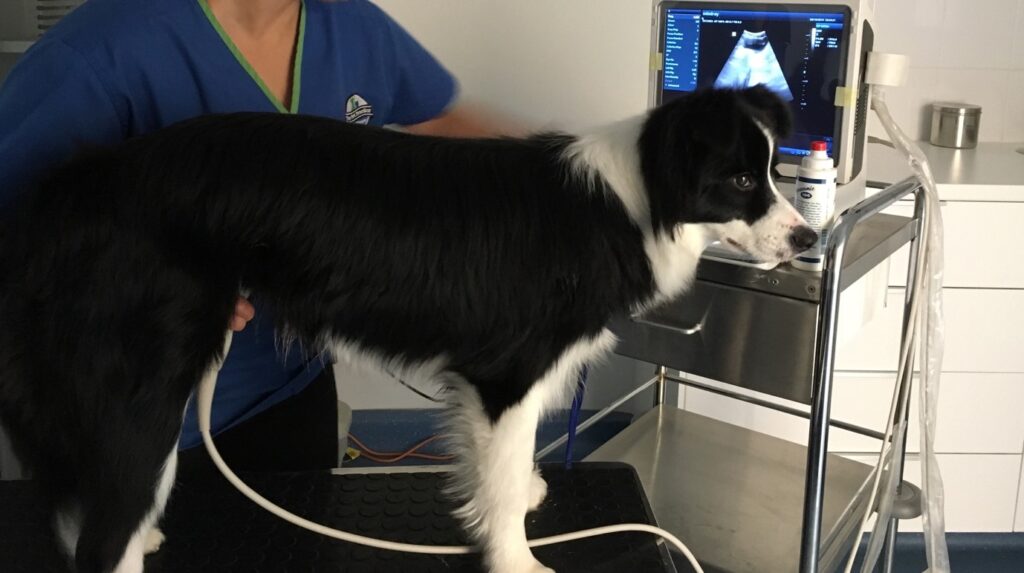
Figure 2: Raven receiving an abdominal ultrasound to check the pancreas for signs of inflammation.
Pancreatitis cannot be diagnosed on one sole lab test alone, but several steps are often required to exclude other potential life threatening causes and increase the suspicion of pancreatitis. To begin with your vet may require:
- a thorough history e.g. diet, medications, pre-existing conditions
- physical examination
- blood tests e.g. complete blood count, biochemistry, inhouse snap test SPEC cPL
- diagnostic imaging e.g. xrays or ultrasound
What does treatment involve?

Figure 3: Raven being hospitalised and treated with intravenous (IV) fluids for rehydration and IV medications.
Treatment for acute pancreatitis is based on supporting recovery and managing complications associated with pancreatitis. Typical measures taken include hospitalisation, intravenous fluid therapy, nutritional support, pain medications, and medications to stop vomiting. Other steps may be taken depending on the state of your dog.
For milder forms of chronic pancreatitis it is worthwhile evaluating your pet further for potential risk factors such as inflammatory bowel disease, liver inflammation, or diabetes mellitus. Further treatments for these diseases may be required.
The next step for any form of pancreatitis is to switch to an ultra low fat diet which your veterinarian can recommend and prescribe for you. This diet must be fed exclusively, your pet must not ingest treats, tid-bits, or scraps. If you must feed treats then they have to be low fat such as vegetables (no onions or garlic), fruits (no grapes or raisins), or commercial low fat treats.
Ongoing care
Initially you can expect regular check-ups with your vet to ensure treatment is working well. Some patients that develop chronic pancreatitis eventually require immunosuppression to control signs. Unfortunately, there are some patients who never recover and continue to worsen despite best efforts by your vet.
